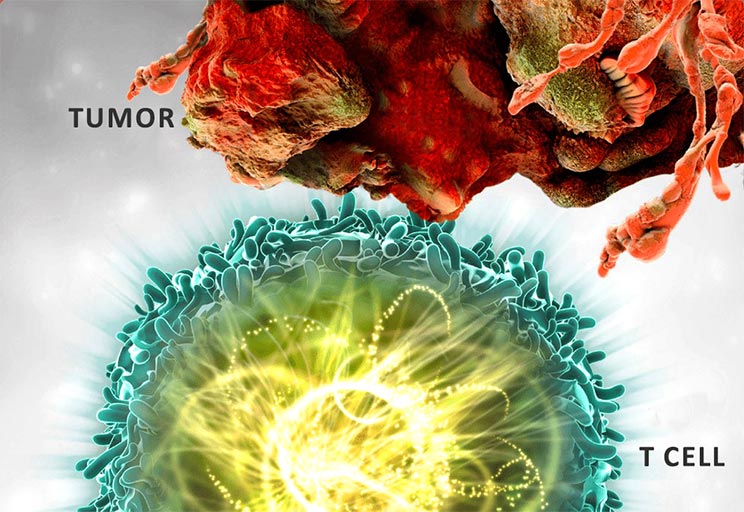
Cancer cases in India are expected to rise 12.8% by 2025 due to mutations in genes that impact, protein expression, and alter cells. Chimeric Antigen Receptor T cells (CAR-T) are genetically modified fusion proteins that can be expressed and transfused into patients. CAR-redirected T cells offer a promising cell-based immunotherapy method that can enhance and maintain antitumor GVL response without major histocompatibility complex restriction. The structure of CARs includes an intracellular signaling domain, a transmembrane domain, and an extracellular domain. The importance of single-chain variable fragment (scFv) in CAR-T cell therapy is due to their complete antigen-binding capability, which allows for faster and more even penetration to tumors and other tissues. Five generations of CAR-T cells have been created since 1989, with the first generation having limited expansion and persistence due to lack of a costimulatory signal. The manufacturing process for CAR T cells involves stimulating, transducing, expanding, and cryopreserving T cells under Good Manufacturing Practices conditions. This blog describes the evolution and brief applications of approved CART cell therapy.